Diabetic Retinopathy
 Diabetic retinopathy includes a number of changes in the retina which can develop as a result of diabetes (either type 1 or type 2). The earliest signs are small red dots in the retina called microaneurysms which represent small pouches on the smallest retinal blood vessels called capillaries. These microaneurysms can leak fluid from the blood stream (serum) into the retina which can lead to swelling in the retina (macular edema). Later, retinal hemorrhages and white spots called cotton-wool spots may develop in the retina. With more advanced retinopathy, small irregular capillaries may develop called intraretinal microvascular abnormalities (IRMA) and venous beading where the retinal veins will have areas of dilation next to areas of normal blood vessel caliber. All of these changes are called non-proliferative diabetic retinopathy. Some eyes advance to proliferative diabetic retinopathy which is characterized by the development
Diabetic retinopathy includes a number of changes in the retina which can develop as a result of diabetes (either type 1 or type 2). The earliest signs are small red dots in the retina called microaneurysms which represent small pouches on the smallest retinal blood vessels called capillaries. These microaneurysms can leak fluid from the blood stream (serum) into the retina which can lead to swelling in the retina (macular edema). Later, retinal hemorrhages and white spots called cotton-wool spots may develop in the retina. With more advanced retinopathy, small irregular capillaries may develop called intraretinal microvascular abnormalities (IRMA) and venous beading where the retinal veins will have areas of dilation next to areas of normal blood vessel caliber. All of these changes are called non-proliferative diabetic retinopathy. Some eyes advance to proliferative diabetic retinopathy which is characterized by the development 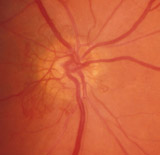 of new, fragile blood vessels on the surface of the optic nerve or retina. These abnormal blood vessels are called neovascularization and have a tendency to bleed into the vitreous cavity causing a vitreous hemorrhage. The neovascularization may also cause scar tissue to form on the retina which can pull on the retina leading to traction retinal detachment. Sometimes, neovascularization also grows in the front of the eye on the iris which can lead to a very severe form of glaucoma.
of new, fragile blood vessels on the surface of the optic nerve or retina. These abnormal blood vessels are called neovascularization and have a tendency to bleed into the vitreous cavity causing a vitreous hemorrhage. The neovascularization may also cause scar tissue to form on the retina which can pull on the retina leading to traction retinal detachment. Sometimes, neovascularization also grows in the front of the eye on the iris which can lead to a very severe form of glaucoma.
Warning symptoms of diabetic retinopathy
Many people with non-proliferative and proliferative diabetic retinopathy have normal vision, especially if vitreous hemorrhage or traction retinal detachment is absent. This is why regular eye examinations are essential since treatment is most effective before eyes lose vision. Blurred vision is the most common symptom caused by diabetic retinopathy. Another important symptom is the sudden onset of floaters which can be due to a vitreous hemorrhage.
What causes diabetic retinopathy?
Diabetic retinopathy is primarily caused by damage to the retinal blood vessels as a result of elevated sugar (glucose) levels in the bloodstream. The normal retinal blood vessels are damaged by chronic elevated glucose levels and may begin to leak fluid or cause small hemorrhages in the retina. In more advanced stages of diabetic retinopathy, the retinal blood vessels become occluded leading to inadequate oxygen levels in the retina. The retina sends out a signal to grow new blood vessels and abnormal vessels called neovascularization form.
Treatment of diabetic retinopathy
The first goal of diabetic retinopathy treatment is to control blood glucose. Good control of blood glucose helps to slow the development and progression of diabetic retinopathy although is does not prevent the diabetic retinopathy altogether. Diabetic macular edema is treated with laser photocoagulation which places small burns around the central part of the retina called the macula or with injections of drugs such as ranibizumab, bevacizumab or steroids into the eye (intravitreal injections). The preferred treatment is determined by the severity and location of the macular edema. These intravitreal injections must often be repeated to control the macular edema. Proliferative diabetic retinopathy is treated primarily with laser photocoagulation where laser burns are placed in the peripheral retina. This helps to decrease the oxygen demands of the retina which causes the retinal and disc neovascularization to resolve or decrease. The laser procedures and intravitreal injections are typically performed in the office. Some eyes which develop vitreous hemorrhages or traction retinal detachments require a surgical procedure called a vitrectomy which is performed in an operating room. The key to successful treatment of diabetic retinopathy is early detection so it can be treated at earlier stages rather than later stages. Often vision loss from diabetic retinopathy can be prevented with appropriate and timely treatment.
